If we go back to post 5 which deals with circulation in the unborn baby we will remember the 'ductus arteriosus' which is a very important structure in fetal life. It is through the ductus that blood circulates through the lower half of the baby. Usually the ductus arteriosus closes spontaneously after birth due to the effect of oxygen in the air that the baby breathes in. Closure of the ductus can take anywhere between 24-72 hours
In some babies the ductus does not close and can remain open resulting in Patent ductus arteriosus (PDA). If the PDA is small it may be of little consequence and sometimes can even be left alone. If however it is sizable it can lead to increased blood flow to the lungs which can cause breathlessness, poor feeding, sweating, poor weight gain etc in the baby. If left untreated in the long-term it can give rise to high pressure in the lungs (pulmonary hypertension)
PDA is commonly found in premature babies and also in babies of mothers who have had Rubella infection.
Timing of treatment depends on the size of the PDA. If the PDA is large it will need early treatment. If small it can be observed till 9-12 months of age giving time for spontaneous closure. PDA usually does not close spontaneously beyond the age of 1 year.
Treatment of PDA may be
(a) Medical: This is possible in preterm babies where certain drugs (NSAIDS like brufen or indomethacin) can be given to try and close the PDA. This has to be undertaken under the careful supervision of a children's doctor in hospital.
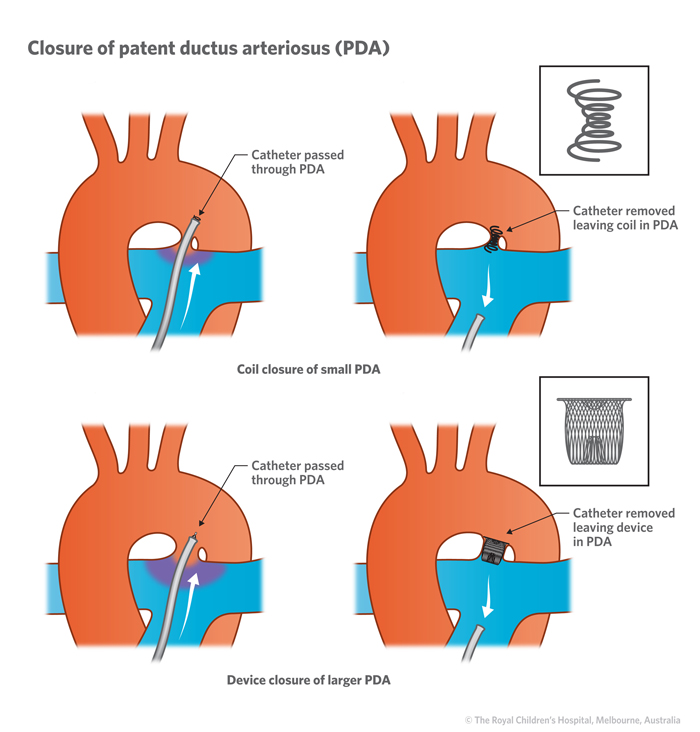
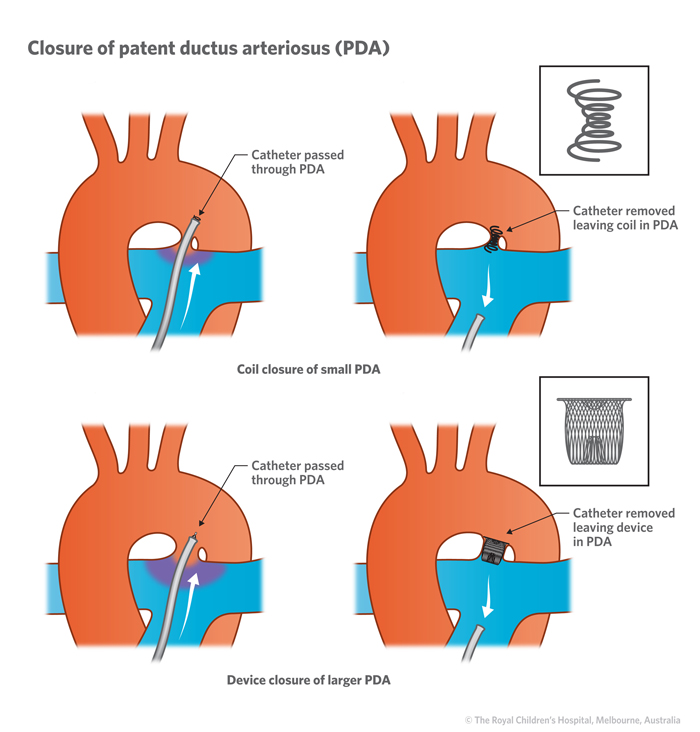
(b) Key hole: Here the PDA is closed using a button device. The device is introduced from the leg and inserted without open surgery across the PDA to close it. This technique may not be suitable for very larger PDAs in small babies.

(c) Surgery: This involves opening the chest and cutting and tying the PDA to eliminate it. This usually involves a longer hospital stay than key hole treatment.
Following successful elimination of the PDA the heart is essentially normal and we expect the patient to have a normal childhood and adult life.
In some babies the ductus does not close and can remain open resulting in Patent ductus arteriosus (PDA). If the PDA is small it may be of little consequence and sometimes can even be left alone. If however it is sizable it can lead to increased blood flow to the lungs which can cause breathlessness, poor feeding, sweating, poor weight gain etc in the baby. If left untreated in the long-term it can give rise to high pressure in the lungs (pulmonary hypertension)
PDA is commonly found in premature babies and also in babies of mothers who have had Rubella infection.
Timing of treatment depends on the size of the PDA. If the PDA is large it will need early treatment. If small it can be observed till 9-12 months of age giving time for spontaneous closure. PDA usually does not close spontaneously beyond the age of 1 year.
Treatment of PDA may be
(a) Medical: This is possible in preterm babies where certain drugs (NSAIDS like brufen or indomethacin) can be given to try and close the PDA. This has to be undertaken under the careful supervision of a children's doctor in hospital.
(b) Key hole: Here the PDA is closed using a button device. The device is introduced from the leg and inserted without open surgery across the PDA to close it. This technique may not be suitable for very larger PDAs in small babies.
(c) Surgery: This involves opening the chest and cutting and tying the PDA to eliminate it. This usually involves a longer hospital stay than key hole treatment.
Following successful elimination of the PDA the heart is essentially normal and we expect the patient to have a normal childhood and adult life.